- Recognize the need for planning around children with special health care needs like asthma and allergies.
- Describe your program’s policies regarding medication and individual care plans.
- Provide a healthy environment for all children by following procedures related to allergies, medication, and care plans.
Learn
Know
Children will enter your care with a variety of needs. All programs must be prepared to serve children with allergies, asthma, diabetes, health impairments, physical disabilities, and more. This lesson will help you follow a plan for meeting these children's needs. It also includes strategies for addressing common health concerns.
Each child who enters the program with an identified health care need should have an individual care plan in place. This care plan is developed by a primary care provider and the family. It will give you information about how to care for the child and signs or symptoms to watch for. It is your job to work with the family to put the plan in place.
A care plan typically includes information like:
- The child's diagnosis or diagnoses
- Contact information for the primary care provider (doctor)
- Medications along with the schedule in which the medicine should be given
- Medications to be given on an as-needed basis along with clear instructions about signs and symptoms that warrant giving the medication
- Procedures for administering medications
- Allergies
- Modifications necessary for the child (diet, activity, environment, behavioral, what to avoid--for example, peanuts, etc.)
- Symptoms to look for
- Emergency response plan
- Special training you might need to work with the child
Source: Caring for Our Children (2019)
It may be helpful in some cases for you or your program to communicate with the family and the child's primary care provider. Remember, any communication and information gained is confidential and protected by the Family Educational Rights and Privacy Act (FERPA) and the Health Insurance Portability and Accountability Act (HIPAA). Be familiar with these regulations and ask for help if you need it; refer to your program's guidelines and policies regarding who should talk with the child's primary care provider. A health care consultant can be a good resource.
Always remember that safety is the number one priority for all children and staff. If at any point you have questions or concerns about a child's care plan, speak with your supervisor or the family involved.
Common Health Care Needs
The most common health care needs among school-age children are allergies and asthma. The following information will provide you an overview of each health care need, what to watch for, and ways to support children with these needs. This information can benefit all school-age children because the onset of asthma or certain allergies can develop at any age.
Allergies
Allergies are one of the most common health care needs in children. Allergies can cause a wide variety of symptoms and include an even wider set of causes. According to the American Academy of Pediatrics (AAP), allergies are "reactions that are usually caused by an overactive immune system. These reactions can occur in a variety of organs in the body, resulting in diseases such as asthma, hay fever and eczema. During an allergic reaction, the immune system overreacts and goes into action against a normally harmless substance, such as pollen or animal dander. These allergy-provoking substances are called allergens. As a school-age staff member, you should be aware of allergens that children in your care have, their common symptoms and reactions to these allergens, and what you can do to make your program's space allergy-friendly.
Allergies can be difficult to diagnose and can develop at any age. A child may not have any allergy symptoms at age 6, but by age 8 they could develop a severe allergy. This is one of the reasons why it is important to monitor the health of the children in your care. If you have concerns that a child may have an allergy, bring it to the attention of your coach, trainer, or administrator and the child's parents.
Food Allergies
According to the American Academy of Pediatrics, 8 percent of children under the age of 18 have a food allergy or multiple food allergies. This is roughly 6 million children in the U.S. (AAP, 2011). Various proteins, harmless to people without allergies, can trigger serious reactions in people with food allergies. The reactions can range from mild to severe, including death. Allergic reactions usually happen shortly after the food is eaten.
Recent scientific and medical advances have provided the technology to diagnose food allergies more easily and precisely. We now know that many children suffer from food allergies, some of which can be severe, even life-threatening. Eight foods or food groups account for most serious allergic reactions in the United States: milk, eggs, fish, crustacean shellfish, wheat, soy, peanuts, and tree nuts (Centers for Disease Control and Prevention, n.d.). For example, we have seen an increase in children with peanut allergies, so much so that entire classrooms and care environments have become peanut free zones in order to prevent serious allergic reactions.
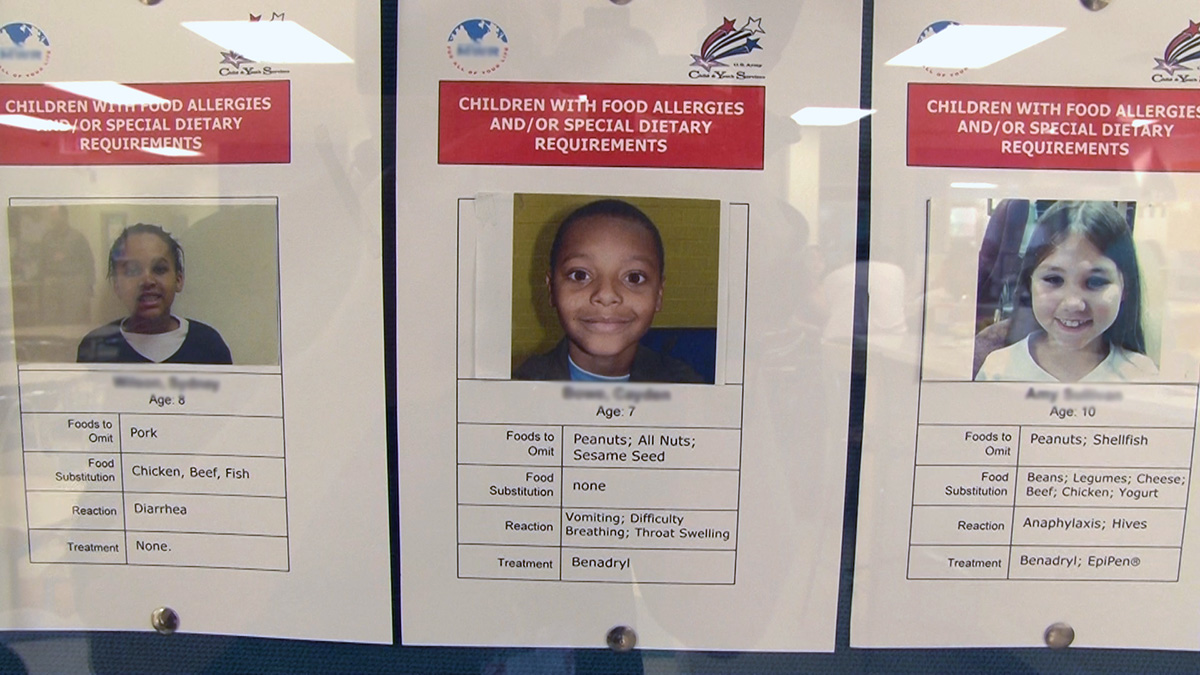
By the time children reach school age, they will more than likely be aware of any food allergies they have and know what foods they can and cannot eat. It is still important, however, for you to know if any school-agers in your care have food allergies. A list of documented allergies should be posted in your program. Stay vigilant at mealtimes to ensure children are not exposed to foods that contain known allergens. If there is a school-age child with a severe allergy in your care, you, a coach, trainer, or administrator, and perhaps a nurse or health aid, should meet with the family to discuss any medications or emergency plans.
Food allergies can affect many parts of the body. Common symptoms include:
- Hives, skin rashes, and swelling
- Sneezing, wheezing, and throat tightness
- Nausea, vomiting, and diarrhea
- Lightheadedness, and loss of consciousness
If the symptoms are severe or if several areas of the body are affected, the reaction could be life-threatening. If the child has an itchy rash, swelling of the throat, and low blood pressure, they likely have anaphylaxis and require immediate medical attention. If you notice that a child is having an allergic reaction that is severe or out of the ordinary, seek immediate emergency medical attention.
While there are more than 160 types of foods that can cause an allergic response in sensitive individuals, these eight foods account for 90 percent of food allergy reactions:
- Milk
- Eggs
- Fish
- Crustacean shellfish (e.g. crab, lobster, shrimp)
- Tree nuts (e.g., almonds, walnuts, pecans)
- Peanuts
- Wheat
- Soybeans
This topic is explored in greater detail in Lesson Seven of the Essentials in Child Care Food Service course.
Non-Food Allergies
There are many other allergens (manmade and natural) that can cause allergic symptoms like runny nose or sneezing, coughing, wheezing, chest tightness, skin rashes, itchy, and watery or red eyes. Common non-food related allergens include:
- Dust mites
- Animals or animal dander
- Mold
- Pollen (trees, grasses, weeds, flowers)
If you suspect that a school-age child in your care may have an undiagnosed allergy, talk with your coach, trainer, or administrator and with the child's family to discuss the symptoms you notice. If the child is having an allergic reaction to an environmental allergen that is specific to your program, the symptoms may not be as noticeable at home.
Be aware that some school-agers may have animal allergies. Certain class pets may be harmful to such children. All children should wash their hands before and after handling an animal.
Asthma
According to the Centers for Disease Control and Prevention, more than 26 million Americans suffer from asthma—more than 6 million of whom are under the age of 18 (CDC, 2020). As the number of people with asthma continues to rise, more accurate methods are available to diagnose and treat the disease. Asthma can begin at any age; however most children develop symptoms by age 5 (Cleveland Clinic, 2019). The American Association of Pediatricians defines asthma as a chronic respiratory disease of the tubes that carry air to the lungs. These air passages become narrow and their linings become swollen, irritated, and inflamed, making breathing difficult (AAP, 2019).
Asthma can be difficult to diagnose. Although the airways are always irritated and inflamed, the symptoms are not always present, but usually sporadic: sometimes they occur often, but at other times there may be long periods between symptoms. Asthma is often mistaken for other health problems, such as respiratory infection, pneumonia, bronchitis, or a chronic cough. For these reasons, it is important that families and caregivers be alert to the possibility of asthma and seek help if they see any of the following symptoms:
- Wheezing
- Regular coughing
- Tight feeling in chest
- Shortness of breath
Asthma Attacks
Asthma attacks are a scary experience for anyone, but they are particularly frightening for children. A child who is diagnosed with asthma will probably be taught strategies to cope with an attack and given an inhaler. However, it is important that you know how to respond to an asthma attack and how to comfort a scared child. Make sure you know and follow the child's care plan in the event of an asthma attack. If a child has their first asthma attack while in your care, seek emergency medical attention immediately. Do your best to keep the child calm, and encourage them to take slow breaths.
See
Supporting School-Age Children with Special Health Needs
You will likely have school-age children in your program that have been identified as having a special health need. This could range from a mild allergy to a severe physical impairment. Whatever the need may be, it is your job to support all children so that they can participate in your program safely.
Watch this video concerning what happens when a child with an identified health need enters a program.
Special Health Care Needs
The following images are examples of ways to support children with special health needs. It is helpful to post photos and lists of any allergies that children in your care may have.
Do
Allergies to Pets or Food
When a child with food or other allergies enters your program, you must keep the child healthy and safe. As with all special health needs, allergies require a care plan for a child. This plan should include written information about the foods or animals the child is allergic to, a written treatment plan, a training plan for staff, and a plan for storing any medicine. The child's allergies should be clearly and prominently posted in your program's space.
If an allergic reaction occurs while the child is at the program, you should administer the prescribed medicine right away, contact the family, contact emergency medical services if necessary, and encourage the family to contact their primary care provider. Be sure to take a copy of the plan, any medication, and a cell phone with you whenever the child leaves the building on a field trip.
Caring for Less Common Health Needs: Medical Procedures
Occasionally, children with more serious medical needs may enter your program. Their medical needs might include tube feedings, catheterization, suctioning, or checking blood sugars. In these cases, a care plan must be in place from the child's primary care provider. If staff are expected to perform the procedures (and if this is acceptable under state law), the plan must include guidelines for training staff in the procedure. If you feel that the procedure is beyond your expertise or training, talk to your coach, trainer, or administrator to get the help you need.
Administering Medication
Providing medication to a child is a serious event. You must only do so by following your program's policy regarding a child's individual care plan. Follow these Rights to prevent mistakes and accidents:
Seven Rights of Administering Medicine
- Right Medication. Staff administering the medication should check the medication against the signed form to ensure that the name of the medication on the bottle or package matches that exactly on the signed form. Each time the medication is administered, this should be checked. The medication should be kept in its original container.
- Right Child. During certain seasons of the year when multiple children may need medication or when the program has several children enrolled who need medication support (such as for diabetes, asthma, or attention deficit hyperactivity disorder), the risk is increased for improper medication administration. Forms and medication need to be checked to ensure that the right child is receiving the medication. If administration is conducted by staff not directly working in the classroom, this is even more crucial.
- Right Dose. Confirmation needs to be made that the right dose has been measured. An excellent way to double check this point is to use the medication spoon dispensed with the medication by the pharmacy. Medication administration is not the place for guesswork. Any questions should be referred back to the family for clarification.
- Right Time. Timing of the medication should be clearly written on the medication itself and on the signed form. Additionally, staff need to confirm with families when the child arrives as to when the last dose of medication was administered and when the next one is due. This information should be documented according to program policy and practice. Likewise, when the child is picked up by the family, staff should provide written documentation of medication administration.
- Right Route. Medication can be delivered in a number of ways; usually the medication to be delivered by programs is through oral dispensing or through an inhaler. Confirmation of method should be written on the medication itself as well as on the signed form.
- Right Reason. Each time medication is given, the person administering it should assure that the medication is begin given for the right reason (e.g., Tylenol for teething pain, breathing treatment for asthma attack). Consulting the health care plan for the appropriate symptoms can help ensure that the medication is given for the correct reason(s).
- Right Documentation. Each time a child is administered medication, it should be recorded. The staff member who administered the medication should document the administration immediately each and every time after they have provided a dose (after washing hands). This is an incredibly critical step. Without proper documentation, another staff member or the child's family member may not appropriately provide the next dose of medication (e.g., they may provide the next dose too quickly which could cause seriously health implications for the child).
If any of these Rights have not been met, then it is considered a medication error, must be documented, and the family notified. You can read more on these rights of medication administration by reviewing the resource Information from the American Academy of Pediatrics on Medication Administration located below in the Learn Activities section.
Any medication or medical equipment should be safely stored in the classroom, office, or nurse's office. Prescription medications should be in a container that has been labeled by the physician or pharmacist. Over-the-counter medication should be stored in its original package. All medications should be stored according to the directions on the containers or as directed by health care professionals. Some may require refrigeration, while others may not. If a child has severe allergies and might go into anaphylactic shock, they will likely be prescribed an epinephrine auto-injector (EpiPen, etc.). Keep the auto-injector available at all times, including field trips.
Explore
It is important to identify resources in your own program to meet children’s special health needs. Read the scenario in the Meet Aiden activity, and write your answers in the space provided. Then talk to your trainer, coach, or administrator about how you would answer the questions as they pertain to your program.
Apply
In this section you will find two documents that you can use as templates for your own work: a Care Plan for Children with Special Health Needs and an Information Exchange Form for Children with Health Concerns. Use these resources as you learn more about the forms required in your workplace.
You can compare the attached documents with information that already exists in your program related to children’s health care needs. Your program’s Inclusion Action Team (IAT) or Nurse should have a Care Plan Template developed and in use. Review this existing paperwork from the IAT to ensure you have all required information in order to provide appropriate services and accommodations for children with special health needs.
Glossary
Demonstrate
American Academy of Pediatrics. (2018). Allergies & Asthma.
https://www.healthychildren.org/English/health-issues/conditions/allergies-asthma/Pages/default.aspx
American Academy of Pediatrics. (2019). Caring for Our Children, National Health and Safety Performance Standards. American Academy of Pediatrics. https://nrckids.org/CFOC/Database/3.2.1.4 & https://nrckids.org
American Academy of Pediatrics. (2003). Guidelines for the Administration of Medication in School. http://pediatrics.aappublications.org/content/112/3/697.full.pdf+html
Aronson, S. S. (2013). Model child care health policies. American Academy of Pediatrics.
Aronson, S. S., & Spahr, P. M. (Eds., 2002). Healthy Young Children: A Manual for Programs. Washington, DC: National Association for the Education of Young Children.
Centers for Disease Control and Prevention (2018). Health Insurance Portability and Accountability Act of 1996 (HIPAA) https://www.cdc.gov/phlp/publications/topic/hipaa.html#:~:text=The%20Health%20Insurance%20Portability%20and%20Accountability%20Act%20of,being%20disclosed%20without%20the%20patient%E2%80%99s%20consent%20or%20knowledge
Cleveland Clinic. (2013). Asthma in Children. https://my.clevelandclinic.org/health/articles/6776-asthma-in-children
National Association for the Education of Young Children. (2007). Keeping Healthy: Families, Teachers, and Children. [Brochure]. Washington, DC: NAEYC.
National Heart, Lung, and Blood Institute (2020) Asthma. https://www.nhlbi.nih.gov/health-topics/asthma
National Institutes of Health (2008). Asthma: How Asthma-Friendly Is Your Child-Care Setting?
http://www.nhlbi.nih.gov/health/public/lung/asthma/chc_chk.htm
North Carolina Child Care Health and Safety Resource Center, (May 2009). Information available by contacting 800-367-2229.
Ritchie, S. & Willer B. (2008). Health: A Guide to the NAEYC Early Childhood Program Standard and Related Accreditation Criteria. Washington, DC: National Association for the Education of Young Children
U.S Department of Education. (2020). Family Educational Rights and Policy Act (FERPA). https://www2.ed.gov/policy/gen/guid/fpco/ferpa/index.html#:~:text=The%20Family%20Educational%20Rights%20and%20Privacy%20Act%20(FERPA),applicable%20program%20of%20the%20U.S.%20Department%20of%20Education
U.S. Food and Drug Administration. (2021). Food allergies: what you need to know. https://www.fda.gov/food/buy-store-serve-safe-food/food-allergies-what-you-need-know
U.S. National Library of Medicine. (2018). Food allergy. https://medlineplus.gov/foodallergy.html
Washington State Fathers Network. (2019). Bothell, WA: Kindering Center. https://www.fathersnetwork.org/


